Doctors say that cancer patients are not getting proper care
 Getty images
Getty imagesSenior doctors responsible for monitoring cancer care in England and Wales are concerned with NHS services, contributing to NHS services, more than half of patients are not getting the right treatment for some cancer.
In evidence provided to BBC, National cancer audit associate center (natakan) Highlights special problems with prostate, kidney and colon cancer.
The expert group stated that it has found significant changes between hospitals and warned the problems reaching the nationally recommended treatments that they are putting life at risk.
It audits in nine major cancer – responsible for 80% of cases – and a range of different cancer types and stages has been found to have been found.
Statistics shared with BBC show:
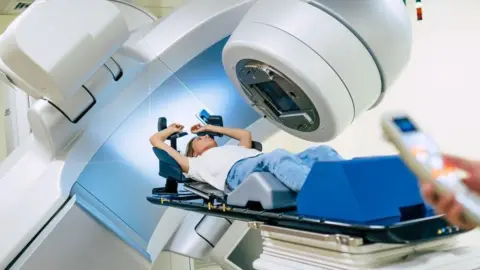
- 30% of patients with high -risk prostate cancer do not get curative treatment with surgery or radiotherapy, with performance vary between 20% and 43% in various services.
- 34% stages of three colon cancer cases do not get chemotherapy within three months of surgery – the number in some hospitals is more than 60%.
- 50% phase four renal cell carcinoma patients, a type of kidney cancer that has spread to other parts of the body, does not get drug treatment – performance with performance varies between 20% and 85%
Natakan said that while a minority of patients does not want to treat themselves and others may not be well enough, which could not fully explain the scale of shortage or variation between hospitals.
Governments of both nations say that improvement in services is an important priority and England is in the process of making a new cancer strategy, which the ministers say that the services will bring revolution.
‘I’m lucky’
The case of Ian Pattison highlights the value of obtaining the right treatment. He was detected at the age of 65 in 2020 at the age of 65.
It began to spread in nearby organs and was offered national-inflammatory treatment of hormone therapy and radiotherapy for their special types of cancer.
He said that treatment was cruel, but now at the age of 70, he is in cancer discounts and is enjoying life.
Mr. Patisson of Durham said: “I was lucky that I live close to an expert cancer center in Newcastle where I could get the best treatment.
“It was going through everyone and competing with side effects, but I am very grateful that I got treatment.
“I feel fit and well. I like to walk, spend time with my family and take care of grandson.”
huge difference
But the clinical director of Natken, run by the Royal College of Surgeons (RCS) for NHS England and Welsh Government, Prof. To understand.
“We need to do better,” he said. “With cancer, we often hear people talking about what the next success is but, the fact that we can make a lot of difference from using what we have better. It will increase life and life Will save. “
Progwal said that there was a possibility of many reasons for problems and variation, in which some services wrongly believe that older patients cannot withstand treatment, as well as problems with staffing and capacity.
He said that there was evidence of small hospitals that patients are not always mentioned at expert centers, where they can get treatment, but also said that some big centers were also coming down for some cancer.
But he said that problems were not uniform with a treatment rate for some cancers types.
RCS president Tim Michel said that the concerns echoed: “NHS has access to world class cancer treatment and care, but inconsistent distribution means many patients are remembered.
“The worst, this may mean that some patients are unnecessarily dying or unnecessary pain.”
dizzy
And the cancer charities stated that the waiting time to deal with failures was definitely more important than reducing the time.
From Macmillan Cancer Support, Eve Biren said that the conclusions were “quite shocking”, saying that dealing with variation in the upcoming national cancer strategy should be “number one priority”.
He said, “To give you the biggest opportunity to survive, one should not come down to get the best care of which hospital you attend or you live in the country,” he said.
Ms. Bayran said that patients should take proper care for their special types of cancer, even where they are.
“We are worried that people from deprived, rural or caste -diverse communities may be particularly lost,” he said.
Amy Raylance from Prostate Cancer UK said that patients were effectively denied their “best opportunities for treatment”, saying: “It needs to be changed now.”
Professor Peter Johnson, director of NHS England Cancer, said: “We know that the experience of cancer of patients is often different – and we are working hard to address it.”
And a spokesperson for health and social care said: “Patients should be able to use cancer care, where they live, where they live and we are committed to addressing health inequalities because we rebuild NHS We do.”
A new cancer strategy is expected to be published in the second half of the year, which Health Secretary Wes Streeting has said that the services will bring revolution.
A spokesman for the Welsh government said that he was working with NHS to “plan, distribute, recover and improve cancer services”.
He said that the audit highlights the areas where further work was needed.



