First gene-editing therapy to treat blood disorder
 Keerthana Balachandran
Keerthana BalachandranThe first therapy to use gene-editing will be offered to patients on the NHS in a “revolutionary breakthrough”.
It will be used as a possible treatment for the blood disorder beta thalassemia.
The blood-forming stem cells would be extracted, reprogrammed to correct the condition, and returned to the patient’s body.
This will save them from needing a blood transfusion every three to five weeks for the rest of their lives.
People with beta thalassemia have difficulty making enough hemoglobin, a protein found in red blood cells that carries oxygen throughout the body.
It is a genetic disease that passes through families and is caused by a defect in the body’s instructions for making hemoglobin.
This can cause people to suffer from severe fatigue, weakness, breathing difficulties and may also reduce life expectancy.
Keerthana Balachandran, 21, was diagnosed with the disease when she was just three months old. She suffers from muscle and back pain and her heart rate increases when she walks uphill.
“The thought of being dependent on blood transfusions for the rest of my life is scary; I am constantly worried about the future,” she says.
The idea of gene-editing is that you only have to do it once.
‘I feel reborn after pioneering gene-editing treatment’
Two women win chemistry Nobel in historic win
How does gene-editing work?
It relies on a tool called CRISPR, which won the Nobel Prize for Chemistry in 2020. It is essentially a satnav attached to a pair of scissors – one part of it targets the right part of the DNA and the other does the editing.
You might be thinking that this technology is being used to fix genetic defects, but it’s actually much more fascinating than that.
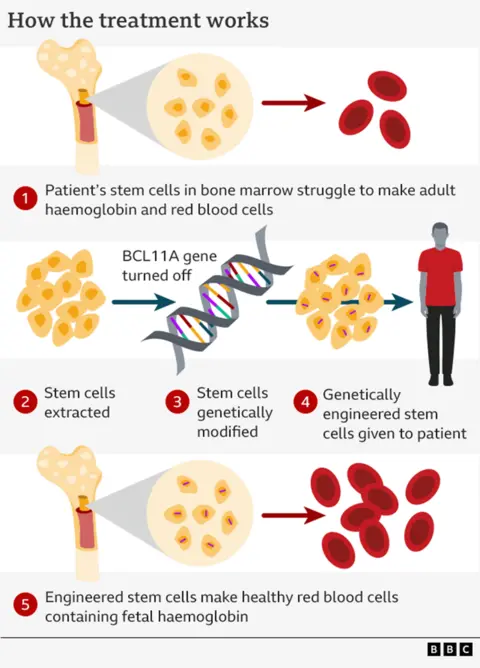
Instead, it depends on the fact that your body makes different types of hemoglobin before and after birth.
When we’re in the womb, our bodies use “fetal hemoglobin” to draw oxygen from our mother’s bloodstream.
When we’re born, a genetic switch turns on and we begin making “adult hemoglobin.”
Importantly, only adult hemoglobin is affected by beta thalassemia.
This therapy disables the switch – called BCL11A – allowing the adult body to once again make fetal hemoglobin.
To do this, the stem cells that produce red blood cells in our spongy bone marrow are extracted.
These cells are sent to the laboratory where the genetic switch is targeted.
The next stage is unpleasant. It involves a course of chemotherapy to destroy the old stem cells that were producing the broken down haemoglobin, after which new stem cells can be infused.
Worth £1.6 million?
The National Institute for Health and Care Excellence medicines watchdog has approved the therapy, which it calls a “potential cure”, after assessing the costs and benefits.
A compromise has been reached which means NHS England is paying less than the official price of £1.6 million per patient.
It is estimated that 460 people over the age of 12 will be eligible to receive the therapy if they want it, and it will be made available at seven specialist centres “within a few weeks”.
NHS chief executive Amanda Pritchard said: “This is a historic moment for people with beta thalassaemia, as a potential cure for those suffering from this debilitating disease is now available on the NHS.”
Beta thalassemia mainly affects people of Mediterranean, South Asian, Southeast Asian, and Middle Eastern backgrounds.
Previously, the only alternative to blood transfusions was stem cell transplantation, but this was rare as it required a very close match of the donor’s tissue.
Casgabi, developed by the Vertex company, is the first approved therapy to use CRISPR-technology.
Romain Maharaj, executive director of the UK Thalassaemia Society, said “we are on the verge of a revolutionary breakthrough” and “this is a ray of hope”.
Talks are still ongoing over whether the same therapy could be used in the NHS for another genetic disease affecting haemoglobin – sickle cell anaemia.



