Jackie Shroff urges couples to get tested for thalassemia before planning pregnancy; Here’s why it’s important
In a recent conversation with YouTuber Ranveer Allahbadia, actor Jackie Shroff emphasises the need for couples to get tested for thalassemia, a genetic blood disorder. Shroff explains the importance of testing for thalassemia even before pregnancy, as both parents being carriers can cause serious health problems to their child, including the need for lifelong blood transfusions. Read on to know more.
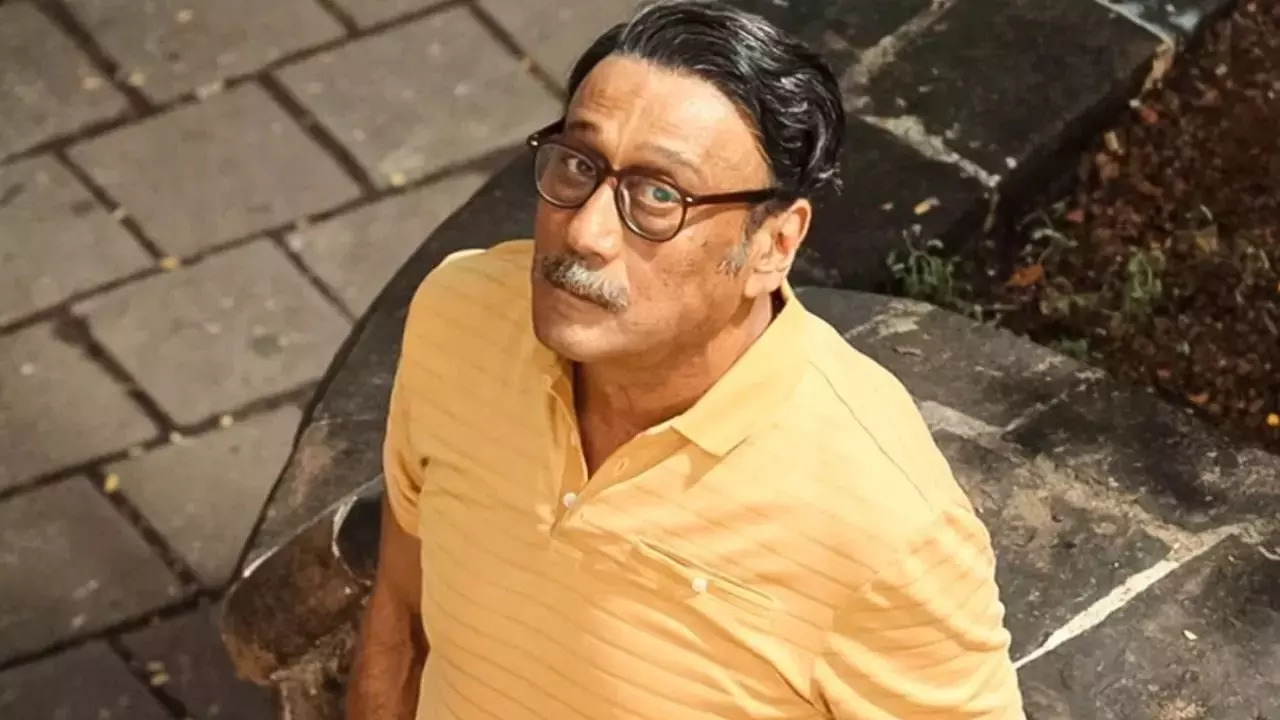
Jackie Shroff urges couples to get tested for thalassemia before planning pregnancy – find out why (Image credit: Instagram)
bollywood actors Jackie Shroff raising awareness about ThalassemiaA serious blood disorder. In a recent conversation with YouTuber Ranveer AllahabadiaShroff emphasised the importance of understanding and discussing thalassemia, especially before planning a pregnancy. “Awareness about thalassemia is very important,” said Shroff. “Everyone should get tested for it. If both parents have thalassemia minor, there is a risk of the child having thalassemia major, which means the child will need a blood transfusion every 15 days throughout their life.” But what is thalassemia? How does it happen? Let’s find out!
What is Thalassemia?
Thalassemia is a genetic blood disorder that is passed from parents to children. It occurs when the body is unable to produce enough hemoglobin, an important protein found in red blood cells. Without enough hemoglobin, red blood cells cannot function properly and have a shorter lifespan, reducing the number of healthy red blood cells in the bloodstream.
Red blood cells are responsible for delivering oxygen to all the cells of the body, which they depend on to function. When there are not enough healthy red blood cells, less oxygen reaches the body’s cells, causing symptoms such as fatigue, weakness, and shortness of breath. This condition is known as anemia, which can range from mild to severe in people with thalassemia. Severe anemia can lead to organ damage and, in severe cases, can be life-threatening.
Types of Thalassemia
Thalassemia is caused by mutations in the genes responsible for hemoglobin production. These mutations are inherited from parents and result in a reduction or absence of one of the hemoglobin chains: alpha or beta. Depending on which hemoglobin chain is affected, thalassemia is classified into two main types: alpha-thalassemia and beta-thalassemia.
Alpha-thalassemia: This occurs when the alpha-globin gene is affected. People with one or more mutated genes may have a mild form of the disease, while people with mutations in all four genes usually have a more severe form of the condition.
Beta-thalassemia: caused by mutations in the beta-globin gene. Depending on the number of mutated genes inherited, it can be thalassemia minor (one mutated gene) or thalassemia major (two mutated genes), the latter being the more severe form of the disorder.
Symptoms of Thalassemia
People with thalassemia minor have few or no symptoms and often lead normal lives. However, people with thalassemia major or other more severe forms of the disorder may have a variety of symptoms, including:
Severe anemia: Fatigue, weakness, and shortness of breath due to a lack of oxygen in the blood.
Pale or yellowish skin: Due to the breakdown of red blood cells.
Delayed growth: In children, due to the body’s inability to produce enough healthy red blood cells.
Bone deformities: Especially in the face and skull, as the bone marrow expands in an attempt by the body to produce more red blood cells.
Enlarged spleen: Due to accumulation of damaged red blood cells.
Frequent infections: Due to a weakened immune system associated with anemia.
Diagnosis of Thalassemia
Thalassemia is usually diagnosed through a combination of blood tests and genetic testing.
– Complete blood count (CBC): This test measures hemoglobin levels and the number of red blood cells, helping to identify anemia.
– Hemoglobin electrophoresis: used to analyze the different types of hemoglobin present in the blood and to detect abnormal forms.
– Genetic testing: confirms the diagnosis by identifying mutations in the alpha or beta-globin genes. This is particularly useful in determining the carrier status of parents and assessing the risk of passing the condition on to offspring.
– Prenatal testing: For expectant parents, prenatal testing can detect whether the fetus has thalassemia, allowing early intervention if needed.
Treatment of Thalassemia
Treatment for thalassemia depends on the type and severity of the disorder. While thalassemia minor often requires no treatment, more severe forms require ongoing medical care.
– Regular blood transfusions: The primary treatment for individuals with severe thalassemia (such as thalassemia major) is regular blood transfusions, which help maintain healthy levels of red blood cells and hemoglobin. These transfusions are usually needed every two to four weeks.
– Iron chelation therapy: Frequent blood transfusions can lead to excess iron in the body, which can cause organ damage. Iron chelation therapy helps remove this excess iron to prevent complications.
– Folic acid supplements: Folic acid is often prescribed to aid in the production of red blood cells.
– Bone marrow or stem cell transplant: In some cases, a bone marrow or stem cell transplant may be considered. This procedure, which involves replacing the defective bone marrow with healthy marrow from a donor, is currently the only possible cure for thalassemia. However, it is not suitable for all patients because of the risks involved.
Get the latest news on Times Now as well as breaking news and top headlines from across health and the world.


