‘Mom is dying and it can be stopped’
 family gift
family giftThe family of a woman who took her own life after suffering postnatal depression for the second time say she was ‘let down’ by mental health services.
Lucy struggled with her mental health after the birth of her first child, but her family say she was not given any extra support when the depression returned after the birth of her second child.
They are calling on the Government to end the postcode lottery on perinatal mental health care.
‘It’s like a living nightmare’
Lucy died on 23 September after disappearing from a psychiatric unit in Scarborough, where she was living as a voluntary patient.
After hours of searching with mountain rescue, her sister Faye was told that the “bubbly, caring and talented mother” had taken her own life.
“I just screamed. It was incredible. It’s like a living nightmare for the whole family,” Faye said. “Their three-year-old is still asking when mummy is coming home and pointing at mummy on the side of the bed.”
But Lucy’s death was not sudden.
 family gift
family giftWhen Lucy’s first child was three months old, she began suffering from postpartum depression.
“She changed massively. A dark cloud came over him and took away his entire life,” Faye said.
“Any joy he had taken from life was gone. His anxiety was sky high. His depression was terrible. Insomnia and fatigue – it took over his life.”

Her parents brought Lucy and the baby into their home, she was given antidepressants and around the time their daughter turned one, she began to recover.
“Lucy came back to us and she was wonderful”, said her mother Ann.
Lucy told her family that she did not recognize the person she was when she suffered from depression.
 family gift
family giftWhen Lucy became pregnant with her second child in 2023, her family were shocked to learn that no additional support was provided.
“I assumed more care would be needed, knowing this was the first time she had had depression. But no additional support or care was offered”, Faye said.
His family says that the first three months after the birth of their son were wonderful.
“She was a wonderful mother. Very creative. She did everything for her kids”, Faye said.
But again, depression struck when her baby was three months old, and despite her family’s best efforts she said it was even worse this time.
“We were flailing. We also needed help. We gave him medicine and it was being changed continuously. It wasn’t working,” Ann said.

Lucy began to talk seriously about taking her own life and her husband contacted the crisis mental health team.
She received some counseling and home visits, and was then referred to an antenatal team who provided weekly counseling sessions.
But due to staff illness, face-to-face sessions were replaced by phone calls and his condition worsened.
In August he attempted to commit suicide. She also began hearing voices, a sign of psychosis that could be the result of severe postpartum depression.
 family gift
family gift“We were all absolutely scared at this point. We were so lost and scared about how we could support him, knowing what he had done,” Faye said.
Lucy was admitted to a psychiatric unit on a voluntary basis, which meant she could come and go freely.
She was given the option of finding a bed in the mother and baby unit, but turned it down, which Faye considers a warning sign.
“She should have been isolated and automatically sent to the mother and baby unit,” he said.
“If the mother doesn’t feel like she wants to be with her baby, alarm bells should be ringing.”
Eight days before she died, Lucy wrote in her hospital journal, “Help me”.
 family gift
family giftOn the day Lucy died her mother visited her in hospital and took her out for lunch. This was the last time she saw her daughter alive – Lucy never returned to the hospital or home to her children.
“No child should ever ask why his mother is not coming home. No husband can live without his wife. And no parent should have to bury their daughter for something that is treatable,” Faye said.
 family gift
family giftLucy’s death is part of a bigger picture.
The postcode lottery of perinatal services is stark. Yet according to the NHS one in 10 women suffers from postnatal depression.
Research from the Maternal Mental Health Alliance (MMHA) shows that North Yorkshire, where Lucy lived, did not meet the care quality standards for antenatal care set by the Royal College of Psychiatrists 2023.
The orange parts of the map highlight areas where there are shortages of staff and services.
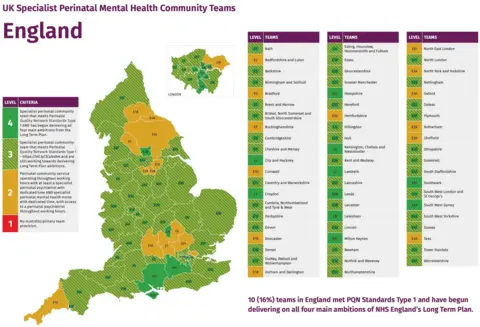 Maternal Mental Health Coalition
Maternal Mental Health CoalitionKaren Middleton, head of policy at the MMHA, says mothers are failing because of a lack of consistent maternal mental health care.
“Maternal mental health is not fully understood and has historically been underinvested in,” she said.
“We need to raise awareness so that commissioners and managers at local level provide sustainable funding that is based on the level of need in their area.”
According to the latest Saving Lives, Improving Mothers Care (SLIMC) report, maternal suicide is the leading cause of direct death of mothers when babies are between six weeks to one year old.
This is unchanged since 2009.
Care is under review
A spokesperson for Tees, Esk and Wear Valleys NHS Foundation Trust said: “Our thoughts are with Lucy’s family and friends.
“We are keeping a close eye on the care Lucy received from us and, taking into account national guidance, we will establish whether we could have done anything differently to prevent Lucy’s death.
“We will support Lucy’s family through this process as their partnership is incredibly important.”
A spokesperson for NHS Humber and North Yorkshire Integrated Care Board (ICB) expressed his condolences to Lucy’s family and friends, and said it would be “not appropriate” to comment further while the review is ongoing.
The Department of Health and Social Care said it was “unacceptable” that anyone should feel let down by maternity support services.
A spokesperson said, “Specialist perinatal mental health services are established in all parts of England, but we know there is a need for more.”
“Many people with mental health problems, including mothers who have recently given birth, are not getting the support or care they need.
“That’s why we’re reforming the Mental Health Act to fix the broken system and give more people more power over their care.”
 family gift
family giftLucy’s family says she was a victim of the system. But they are committed to fighting for change.
“Mothers are dying and it can be stopped. We have a baby and a three-year-old growing up without his mother,” Faye said.
“We need to save the mummies.”
If you have been affected by any of the issues raised in this story, you can visit bbc action line,
You can also email yorkslincsinvestigations@bbc.co.uk to share your experiences.



