Mother calls 999 to give seriously ill son painkillers due to ambulance delay
 Roisin Wilshaw
Roisin WilshawThe mother of a Belfast man who fainted outside a hospital said she was shocked when a 999 call handler told her she should take painkillers because they would have to wait hours for an ambulance.
Brian Rooney, 35, suffered a heart attack outside the emergency department of the Royal Victoria Hospital after his bowel was punctured at home.
He is now in a coma after emergency surgery, which resulted in his intestine being removed.
The Northern Ireland Ambulance Service (NIAS) apologized to Mr Rooney and his family “for not meeting their expectations in terms of the care provided to them”.
It added that he is “unable to comment publicly on the details of individual matters” but “would welcome the opportunity to discuss the issues raised directly with the family”.
Mr Rooney is in serious but stable condition.
His mother Isobel Benson called 999 after her son felt an “explosion” in his chest and was “screaming in agony”.
A hospital consultant later told him that the perforated bowel meant the organ had “effectively burst and the entire contents of his bowel would have been evacuated throughout his body”.
Mr Rooney also has epilepsy, colitis and arthritis, and has recently been in and out of hospital.
What happened to Brian Rooney?
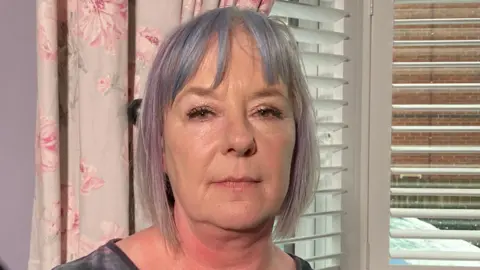
On Sunday morning Ms Benson heard “a loud scream” coming from her son’s attic room.
After seeing the “panic look on his face”, she called for an ambulance.
Ms. Benson said she explained her son’s medical history and told the call handler that he was hyperventilating, in pain and unable to move.
After confirming that he was breathing, lucid and could talk, he was told that it would take a few hours for an ambulance to reach him due to ongoing pressure on the health service.
When Ms. Benson responded that she needed an ambulance now, the call handler asked if she could take her son to the hospital herself.
She said she could not do this because she had a two-door car, which would have been extremely difficult for Mr Rooney to travel in given his level of pain, and her son’s father did not drive at night due to his health problems. Can.
Ms Benson was told she would have to wait and would only be given painkillers.
“After that call I was really in shock. It was just a lack of trust.
“My understanding is what priority call is – if you have severe chest pain, you are given priority, it is an emergency.
“In this case, because they made it clear that it was not considered an emergency, and that was the end of it and it was not up for discussion,” he said.
 Roisin Wilshaw
Roisin WilshawShe said she understood the pressure on the health service, but she never expected the wait for an ambulance to be so long, given her son’s medical history.
“They said the ambulances they had couldn’t release the people they were with, and no one would be available for a few hours,” Ms Benson said.
“This, to me, is communicating that we do not consider you an emergency.”
 Roisin Wilshaw
Roisin WilshawMs Benson said her son now faces an uncertain recovery.
Since his intestine was removed during the surgery, he will now use a stoma to collect waste.
He said his life has been changed, given the rehabilitation and “potential complications such as infection”.
“All these things that we probably don’t know about could have been avoided if the ambulance had arrived on time when I called.”
‘Way above capacity’
Mr Rooney’s case follows reports There are longer wait times in emergency departments during the winter period.
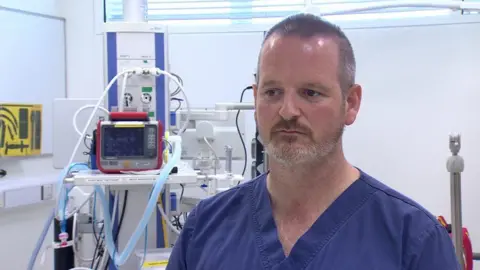
An emergency consultant at Ulster Hospital said the situation there is “dire” and they are currently working well beyond capacity.
Dr Andrew Dobbin, who is clinical director of emergency medicine at the South Eastern Trust, told Good Morning Ulster that there were 690 patients for the hospital’s 540 beds on Tuesday.
He said 100 of them were medically fit to leave the hospital.
Of the 690, 80 were on beds in corridors and another 70 were waiting for beds in the emergency department, which has only 51 rooms.
“There is a huge gap between demand and capacity,” he said.
‘over-capacity’
Dr. Dobbin also said lower use of the flu vaccine this year was a factor.
He said there were “waiting rooms full of vulnerable sick patients”.
He said that then this risk also falls on the working clinical staff.
“Eight out of 16 of our doctors on Monday evening shift were suffering from flu-like illnesses,” he said.
However, he said problems with discharging patients from hospital, as well as how community and social care was provided, was also a major issue.
on tuesday The assembly’s health committee met to discuss the pressure on hospitals in Northern Ireland.



