Why men are so unhealthy – what else can be done
 Getty images
Getty imagesThis month the government in England will start a consultation for its men’s health strategy. This step has long been overdose, experts say that men are more likely to die ahead of time than women. But why are they in such poor health – and what can be done about it?
Andrew Harrison was running a male health clinic from a youth center at Bradford when he heard a knock. He turned to the door, but there was no one. Then he has heard his name. He looked around to see a young man on the window asking for condoms.
“I was on the first floor,” he says, remembering the story from a few years ago. “The child shook a drainpipe outside the building because he did not want to go through the reception and asked.”
Accessories, in many ways, face challenges on men’s health-a combination of risk-taking behavior and lack of confidence and skills to connect with health services.
Initial deaths
Men in the UK are more likely to smoke, drink alcohol, use drugs and high cholesterol and blood pressure.
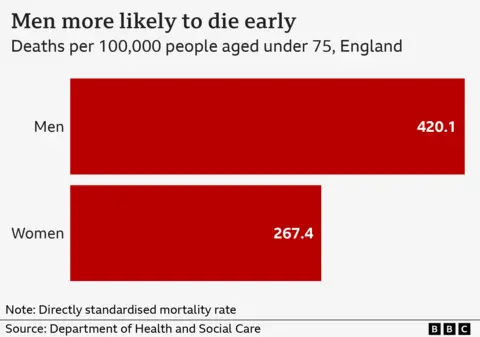
These are the major contributors to the fact that men have a lower life expectancy than women – for four years – and are The probability of premature death is about 60% more than the age of 75 years In heart disease, lung cancer, liver diseases and accidents.
Professor Alan White, who founded the Mains Health Forum Charity and established a dedicated Male Health Center at Leeds Backet University, says the issue needs to be taken more seriously.
He cites epidemics as an example, stating that 19,000 more men died of Kovid, stating that women. “Where was the resentment? Where was the meditation?”
He says that men’s poor health is very easy to blame on their lifestyle, arguing that “it is much more complicated than that.”
He says that there are biological reasons – male immune system is less capable of fighting infection. But, as the story of a young man looking for condoms above, they can also lack skills to reach health services.
Professor White says: “Men are less health-literate, it is to say that they do not develop skills to talk about their health and to identify and act on signals. The health of men is very stable with their teenagers, which in their 40s usually without seeing a health professional in many years.
“It is different for women. Getting contraceptive, screening of cervix and then childbirth means that many women have regular contact with health services in a way, which men do not.”
Clear differences
Machismo is also a factor, Mark Brox, a policy advisor of the All-party parliamentary group on men’s and boys issues, who has played an important role in influencing the government to formulate men’s health strategies.
“We have different expectations about men in society. They are expected to work with things and move forward with things, be strong and flexible.”
But he says that when it comes to men’s health, it is important to pay special attention to the effect of lack. Life expectancy in the poorest 10% regions is 10 years less than the richest – a major difference for women is seen – and in the most disadvantaged areas a man is 3.5 times more of dying before the age of 75 years.
He says, “When you talk about the remaining communities and people working in blue-collar jobs like construction and manufacturing, you cannot ignore clear differences,” they say. “The way health services are designed are not working for men.”
NHS Health checks, which are introduced to people between 40 and 74 years of age every five years, are considered a significant intervention when it comes to many diseases that are claiming men’s lives. But four out of 10 men raise the proposal of less.
“It will be very difficult for someone who is in construction or working on any industrial property to see and look at their GP.”
 Getty images
Getty imagesMr. Brook says that he wants to see employees distributing two hours of time to go for health checkups as well as distributing them in places where blue-collar workers are employed, such as industrial estate.
But he says that it is also an issue about employment – these roles are afraid of facing health problems with some men that develop in the 40s and 50s – ignoring early warnings signs or completely hiding diseases from owners what it can mean for their work.
He says that job anxiety and financial concerns, with relationship problems, is a major driver in high suicide rates seen among men. Three-fourths people who kill their lives are male.
Despite this, only one -third of the men sent for the talk of talking are male, who suggest that services are not enough to consider the needs of men.
Professor White says, “How services are established to identify signs of depression and anxiety, it is not how men express them – they are more likely to display signs of anger, misuse or withdraw alcohol and push people away.”
They say that it is important to identify ethnic differences. For example, black men in England are likely to double with prostate cancer, while men of Indian or Bangladeshi background are particularly at high risk of diabetes.
wake up call
Professor Paul Galdas, a male health expert at York University, says, but it does not mean that men are not interested in their health. “Men will open and engage, but to do so you have to make it a base around tasks and activities.”
He has helped develop a six-week mental fitness program in partnership with the Movember Mens Health Movement tested on the front-line workers of NHS after Covid. It is now being used by Leeds United Football Club for its young players.
Men are provided support to understand how the behavior affects the mood, they are encouraged to track their habits and set goals for healthy activities.
“This can be about developing skills to solve the problem for walking, watching friends, playing golf and protecting mental health. Good mental health leads to good physical health.”
 Getty images
Getty imagesA similar activity-based initiative can be found in many local areas where donations, councils and local men groups have worked together to set up plans.
The male shed movement is probably the most famous where men are encouraged to come together and support each other, while practical projects do.
Professor White says that now is the time to construct these foundations – some national men’s health strategy is important. He says that it would “help shine a spotlight” on this issue in 2022 as a women’s health strategy ” – which created a network of women’s health hubs and women’s health champions in the government’s heart.
But he also wants it to act as a “wake-up call” for men themselves. He says that there are some simple steps that every man should consider.
“Look at the size of your waist – if you are taking weight, if your stomach is too big then try to do something. Go ahead, get out, get out and talk to people.
“Take every opportunity to do health check or check. And, if you are changing the body or the way you are managing problems, seek help.”



